Signs of Gut Health Issues You Should Not Ignore
Benjamin Scott September 28, 2025
Gut health is a growing wellness topic, often linked to digestion, immunity, and mood balance. This guide explores subtle and obvious signs of gut imbalances, the science behind them, and expert-backed strategies for restoring digestive health.
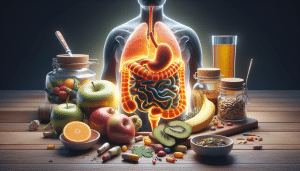
Why Gut Health Matters for Your Whole Body
Gut health extends beyond a comfortable digestive system. The human gut contains trillions of microbes, which play essential roles in breaking down nutrients, training the immune system, and producing vital compounds. When gut bacteria are balanced, nutrient absorption improves, and inflammation stays in check. In contrast, disruptions in the gut microbiome can quickly affect energy, immunity, and mood stability (Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/).
Emerging research also connects gut health to broader wellness topics like mental clarity and the likelihood of developing chronic illnesses. Imbalances, known as dysbiosis, have been linked to autoimmune flare-ups, obesity, and even depression. These findings underscore the gut’s influence across nearly every system in the body and explain why paying attention to subtle digestive symptoms matters for long-term wellbeing.
The microbiome—the genetic material of all microbes in the gut—is personalized. Diet, medications, and stress constantly reshape this landscape. For those experiencing uncomfortable bloating, unpredictable bowel changes, or skin outbreaks, these problems may trace back to gut microbiota. Recognizing signs early allows for lifestyle changes that support better digestion and holistic health benefits.
Common Signs of an Unhealthy Gut
Bloating is one of the most frequently reported signs of gut imbalance. Many people experience occasional discomfort after certain meals, but persistent gas or pain could signal issues with microbial overgrowth or food sensitivities. A sluggish gut may struggle to digest high-fiber foods, resulting in bloating that interferes with daily activities. Identifying triggers often involves a process of tracking symptoms and dietary habits (Source: https://www.gastro.org/practice-guidance/gi-patient-center/topic/abdominal-bloating).
Another classic sign is irregularity in bowel movements. This includes periods of constipation, diarrhea, or even unpredictable switches between both. These fluctuations can arise from imbalances in specific gut bacteria, stress, travel, or medication changes. In some cases, inconsistent digestion points to conditions like irritable bowel syndrome (IBS), highlighting the ongoing relationship between the gut and the nervous system.
Food intolerances also tend to emerge as gut bacteria lose diversity. For example, lactose or gluten intolerance may worsen if bacteria that help break down these substances decrease in number. This can result in uncomfortable cramping, fatigue after meals, and skin flare-ups. Paying attention to recurring issues after consuming particular foods helps in narrowing down underlying gut triggers and fosters proactive management.
Lesser-Known Symptoms Connected to Gut Health
Beyond digestion, unexpected skin changes can be a red flag for underlying gut trouble. Chronic skin conditions like eczema, acne, or unexplained rashes often coincide with digestive complaints. Researchers have linked certain gut bacteria profiles to increased inflammation, which may show up not just in the gut but also on the skin. These indicators invite a closer look at lifestyle habits and gut-friendly practices (Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048199/).
Fatigue is another overlooked symptom that may relate to an imbalanced digestive system. When the gut is under stress, nutrient absorption can decrease, making it harder for the body to get enough energy. In addition, certain harmful gut bacteria can create byproducts that affect the nervous system, leaving individuals feeling sluggish even after a full night’s sleep.
Mood swings and brain fog can also originate from gut issues. The gut produces neurotransmitters, such as serotonin, that support stable mood and cognitive clarity. Dysbiosis may disrupt this production, resulting in irritability, low mood, or difficulty concentrating. Addressing gut health has been linked to improvements in mental wellbeing, which illustrates the power of the gut-brain connection.
Main Drivers of Gut Imbalances
Poor dietary habits are among the strongest contributors to gut microbiome disruptions. Regular consumption of ultra-processed foods, added sugars, and artificial additives lowers microbial diversity, making the gut less resilient. On the other hand, a fiber-rich diet built around vegetables, fruits, and whole grains can help nurture beneficial bacteria (Source: https://www.hsph.harvard.edu/nutritionsource/food-features/gut-microbiota/).
Frequent antibiotic and other medication use has also been shown to disrupt the healthy balance of gut microorganisms. While sometimes critical for treating infections, antibiotics can eliminate entire populations of helpful bacteria alongside harmful ones. This often opens the door for opportunistic pathogens and can set off months of digestive symptoms if not managed thoughtfully.
Chronic emotional stress is an underrated factor in gut health. The gut and brain communicate through the vagus nerve and share neurotransmitters, so ongoing stress can slow digestion or trigger uncomfortable symptoms even when diet remains unchanged. Supportive coping strategies—like exercise, mindfulness, or seeking professional advice—assist in restoring balance throughout both the gut and the central nervous system.
Everyday Steps to Support a Healthy Gut
Restoring gut harmony does not have to be complicated, but does require intention. Dietary changes are foundational—focusing on high-fiber foods, fermented options like yogurt or kefir, and prebiotic-rich choices such as garlic, onion, or asparagus. These changes offer fuel for healthy gut bacteria, encouraging natural balance and resilience (Source: https://www.mayoclinic.org/diseases-conditions/digestive-system-diseases/in-depth/improving-gut-health/art-20460953).
Managing stress is just as critical as managing diet. Daily movement—whether exercise or mindful stretching—supports digestion and reduces tension. Structured relaxation, like deep breathing or guided meditations, can influence the gut-brain axis, supporting smoother bowel activity and reducing stress-related digestive complaints. Practicing consistent sleep hygiene further enhances these effects.
Limiting exposure to unnecessary antibiotics supports long-term microbial diversity. Those advised to use medications can ask healthcare providers about probiotics or other supportive therapies that reduce the impact on the microbiome. Staying informed, reading labels, and experimenting with new, plant-based foods further empower healthy habits for lasting gut balance.
When to Seek Professional Advice for Gut Health
Persistent or severe digestive symptoms may warrant consultation with a healthcare provider. Doctors and registered dietitians can help identify underlying issues—such as celiac disease, inflammatory bowel disease, or food allergies—that mimic common gut imbalance signs but require more specialized management (Source: https://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis).
Diagnostic tests for stool, breath, or blood markers can offer insights into digestion, inflammation, and infection that are not visible through symptoms alone. These tools may guide both dietary recommendations and medical therapies. Reviewing medications and supplement use also ensures that nothing interferes with the efforts to restore gut balance.
A collaborative approach to gut health might include monitoring changes, keeping a food and symptom diary, and staying connected to support networks. With professional input, individuals are better positioned to navigate complex symptoms, avoid unnecessary restrictions, and make lasting lifestyle changes for optimal digestive and overall health.
References
1. Integrative Human Microbiome Project Consortium. (2019). The Integrative Human Microbiome Project. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
2. American Gastroenterological Association. (n.d.). Abdominal Bloating. https://www.gastro.org/practice-guidance/gi-patient-center/topic/abdominal-bloating
3. Salmon, D. M. et al. (2018). The Gut-Brain-Skin Axis: The Link Between Gut Microbiota and Skin Health. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048199/
4. Harvard T.H. Chan School of Public Health. (n.d.). The Nutrition Source – The Microbiome. https://www.hsph.harvard.edu/nutritionsource/food-features/gut-microbiota/
5. Mayo Clinic Staff. (n.d.). Improving Gut Health. https://www.mayoclinic.org/diseases-conditions/digestive-system-diseases/in-depth/improving-gut-health/art-20460953
6. Crohn’s & Colitis Foundation. (n.d.). What Are Crohn’s & Colitis? https://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis