Foods That Can Naturally Support Gut Health
Benjamin Scott September 26, 2025
Curious about how everyday foods could play a role in digestive and immune wellness? Explore insights into what science says about gut health, the impact of nutrition, and simple strategies to nurture a healthy microbiome for overall well-being—all with practical tips and evidence-backed information.
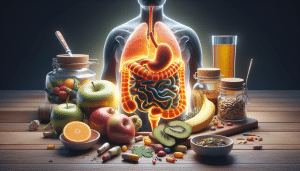
The Importance of Gut Health for Overall Wellness
The connection between gut health and broader wellness has sparked increasing interest. Scientists now recognize the gut as a ‘second brain’ due to its influence on mood, metabolism, and immunity. A well-balanced digestive system can help the body absorb more nutrients from meals, while also providing a protective barrier to unwanted pathogens. Many adults are seeking reliable ways to support their digestive health and enjoy its many ripple effects through diet and lifestyle choices.
The gut houses trillions of bacteria, both beneficial and potentially harmful. These microorganisms form a dynamic community known as the gut microbiome. When in balance, this ecosystem assists in fiber breakdown, vitamin production, and inflammation regulation. However, disruptions—caused by poorly balanced diets, frequent antibiotic use, or chronic stress—can tip the scale, making digestive discomfort or immune challenges more likely.
Research shows that a healthy digestive tract can help support energy levels, mood regulation, and even cognitive function. The gut produces and communicates with neurotransmitters such as serotonin. Supporting gut health is not only about avoiding discomfort but improving daily quality of life. The food choices made each day can influence these processes in significant ways (see: https://www.hsph.harvard.edu/nutritionsource/healthy-gut-microbiome/).
How Fiber Rich Foods Benefit the Digestive System
Fiber is often hailed as an essential nutrient for gut health. Among its many benefits, fiber aids smooth digestion, supports regular bowel movements, and acts as food for beneficial gut bacteria—a process called fermentation. Good sources include oats, whole grains, legumes, fruits, and vegetables. Each type of fiber, whether soluble or insoluble, plays a distinctive role in shaping the digestive environment and helping maintain its balance.
When fiber enters the intestines, it attracts water and bulks up stool, making waste easier to pass. This process not only supports bowel regularity but also helps cleanse the colon. Fermentable fibers—found in foods like apples, beans, and onions—are especially valuable. They are broken down by bacteria into short-chain fatty acids, compounds that further nourish the lining of the colon and support its resilience against irritants.
Research continues to highlight how regular intake of fiber-rich foods is associated with a lower risk of common digestive complaints, including constipation and diverticulitis. Incorporating a variety of fiber types from different plant foods can boost the diversity of the gut microbiome, a marker of digestive wellness. For those new to higher fiber diets, a gradual increase is recommended to allow the gut to adapt comfortably (https://www.cdc.gov/nutrition/data-statistics/know-your-limit-for-added-sugars.html).
Probiotic Foods and Their Role in Microbiome Diversity
Probiotic-rich foods provide living microorganisms that can help tip the balance toward a healthier microbiome landscape. Fermented options such as yogurt, kefir, sauerkraut, kimchi, tempeh, and pickled vegetables are among the most common sources. Introducing these foods to the diet may promote the growth of beneficial bacteria that contribute to efficient digestion, better immunity, and reduced gut inflammation.
The strains of bacteria found in fermented foods differ by the food and preparation method. Yogurt with active cultures and kefir are especially known for containing a high variety of beneficial bacteria. Regular inclusion of such foods has been linked to improved digestion of lactose, decreased symptoms of irritable bowel syndrome, and protection against some infectious organisms. Some people also find that traditional fermented foods can be gentler on the stomach than manufactured supplements.
Probiotic foods are not just about bacteria—many are nutrient-dense, high in protein, or provide vitamins produced as a byproduct of fermentation. These characteristics make them a valuable addition to meals and snacks. When paired with prebiotic foods—those that feed friendly gut bacteria—the effects can be even more pronounced, supporting improved gut diversity and stability (source: https://www.nccih.nih.gov/health/probiotics-what-you-need-to-know).
Prebiotics and the Food Sources That Feed Good Bacteria
In contrast to probiotics, prebiotics are compounds in foods that nourish gut bacteria and help them thrive. They are found in a range of plant-based foods such as onions, garlic, bananas, leeks, asparagus, and Jerusalem artichokes. By adding these fiber-rich vegetables and fruits to the diet, it is possible to naturally support colony growth for a diverse, resilient gut microbiome.
The impact of prebiotic foods extends beyond digestion. As gut bacteria ferment prebiotic fiber, they produce substances that can interact with the immune system and regulate inflammation. Studies suggest this natural process may help reduce risks for certain chronic conditions, while also influencing satiety, energy metabolism, and even skin health. The pairing of probiotics with prebiotics—sometimes called synbiotics—holds extra promise for people with persistent digestive issues.
Diversifying prebiotic sources is key. Eating a broad mix of vegetables, fruits, and grains helps ensure a variety of beneficial bacteria receive what they need to flourish. This approach can help counteract the narrowing of the microbiome caused by highly processed foods or unvaried diets. Maintaining a routine of prebiotic-rich foods makes positive microbial changes more likely to last (reference: https://www.eatright.org/health/wellness/prebiotics-and-probiotics-the-difference-and-their-role-in-your-diet).
Lifestyle Habits That Influence Gut Health
Diet is not the only player in gut wellness. Lifestyle factors—from sleep patterns to exercise—also have a measurable impact on digestive health. Regular physical activity has been shown to encourage a more balanced gut microbiome, helping regulate bowel movement and mitigate stress-induced gut imbalances. Even short activity breaks throughout the day can help support both digestive function and mood.
Sleep quality and circadian rhythms affect gut health, too. Inadequate or erratic sleep patterns are linked to microbiome disruption and lower immunity. Prioritizing restful sleep supports the digestion of food and the repair of gut tissues. Chronic stress creates another challenge, as high levels of stress hormones can change gut bacteria composition and increase the risk of digestive discomfort. Breathing exercises, yoga, and enjoyable hobbies are all strategies that some find helpful.
Another key factor is hydration. Adequate fluid intake assists fiber in moving waste through the intestines. Water also helps maintain the barrier function of the gut lining, shielding the body from toxins and harmful microbes. Those interested in optimizing gut health should approach it as a mix of mindful eating, regular movement, stress management, and hydration—for the greatest overall benefit (https://www.ncbi.nlm.nih.gov/books/NBK279396/).
Common Gut Symptoms and When to Seek Guidance
Occasional digestive symptoms—like bloating, mild cramping, or irregularity—are experienced by many. When these symptoms are persistent, worsen, or disrupt quality of life, they may signal an imbalance or underlying issue. Common red flags include unintentional weight loss, blood in stool, or sudden changes in digestive patterns. It is important to be informed about these signs and review them with a qualified healthcare provider if they persist.
For people with ongoing digestive discomfort, record-keeping can be useful. Tracking meals and symptoms in a journal may help identify triggers or problematic foods. Diverse gut-related conditions exist, and individualized evaluation is vital—gut health is not a one-size-fits-all matter. Standard lab tests and noninvasive procedures can offer key insights into what steps may be most helpful for each individual (see: https://www.gastro.org/practice-guidance/gi-patient-center/topic/gut-microbiome).
When addressing digestive health through food, add new items gradually to observe any response. Some foods that generally benefit gut health may not agree with everyone, especially those with existing allergies or intolerances. Seeking advice from registered dietitians or gastroenterologists ensures that changes are appropriate and aligned with individual health needs (reference: https://www.niddk.nih.gov/health-information/digestive-diseases/digestive-health).
References
1. Harvard T.H. Chan School of Public Health. (n.d.). The Nutrition Source: Healthy Gut Microbiome. Retrieved from https://www.hsph.harvard.edu/nutritionsource/healthy-gut-microbiome/
2. U.S. Centers for Disease Control and Prevention. (n.d.). Know Your Limit for Added Sugars. Retrieved from https://www.cdc.gov/nutrition/data-statistics/know-your-limit-for-added-sugars.html
3. National Center for Complementary and Integrative Health. (n.d.). Probiotics: What You Need To Know. Retrieved from https://www.nccih.nih.gov/health/probiotics-what-you-need-to-know
4. Academy of Nutrition and Dietetics. (n.d.). Prebiotics and Probiotics: The Difference and Their Role in Your Diet. Retrieved from https://www.eatright.org/health/wellness/prebiotics-and-probiotics-the-difference-and-their-role-in-your-diet
5. National Library of Medicine. (n.d.). Nutrition and the Gut. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK279396/
6. National Institute of Diabetes and Digestive and Kidney Diseases. (n.d.). Digestive Health. Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/digestive-health